Complications After Liver Transplant
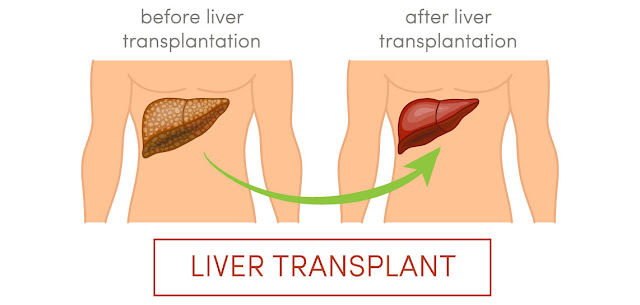
Liver transplant has been advanced as an
operative procedure to substitute the damaged liver of the patient with a
matching liver from a donor, but it still carries a high risk of complications
and side-effects. The following are some of these complications which can be
experienced by the patient who underwent a liver transplant.
§ Ascites
and Fluid Retention
If the patient has a medical history of
ascites and edema or they are malnourished, their chances of experiencing
ascites and fluid retention increases after the liver transplantation. Diuretic
therapy is a common solution to this complication.
§ Biliary
Stenosis
Due to improper dealing of anastomotic
technique, the condition of biliary stenosis can develop in most of the cases.
Biliary stenosis is manifested through cholangitis or persistent abnormal LFT
results. There are certain operative procedures to facilitate the free flow by
unblocking the blood vessel.
§ Bleeding
As per an expert from a renowned institution
of liver transplant in Delhi, the risk of postoperative bleeding is in
the range of 7% to 15% of patients and it is proved by a trustful resource. The
post-operative bleeding can lead to major blood loss which can degrade the
health of the patient to severe levels.
§ Hepatic
artery stenosis and thrombosis
Usually experienced in the early stages following a
liver transplant, hepatic artery stenosis and thrombosis can actually result
into acute massive hepatocyte necrosis, the formation of a central biloma
secondary to intrahepatic duct necrosis, multiple biliary structures, or
intermittent bacteremia.
§ Hepatic
Outflow Obstruction
Due to the risk of morbidity and mortality
linked with hepatic outflow obstruction, transplantation is commonly suggested
to keep the patient safe from life-threatening complications after liver transplantation.
§ Hepatitis
B
Hepatitis B immune globulin (HBIG) and/or
antiviral agents are provided to save the patient from the risk of Hepatitis B. To prevent reinfection. This integrated use of medications has decreased the
risk of Hepatitis B to 10% or even less during the first 2 years post-liver
transplantation.
§ Hepatitis
C
Various factors can amount to reinfection of
Hepatitis C after liver transplantation, including the age and gender of both
the donor and recipient age, the presence of genotype 1, the level of viremia
at the time of transplantation, the use of strong antilymphocyte induction
therapy, and high doses of corticosteroids. Post five years of the liver transplantation,
the risk is less when compared with the first year following liver
transplantation.
§ Infection
It is reported that infection after the liver
transplant is a common and serious complication. Immunosuppressants drugs are
provided to the patient to limit their immune system to react to the foreign
liver from the donor. Also, it is advised by experts of the liver transplant
in India to strictly follow the rehabilitation program and limit the exposure
to infectious agents.
§ Metabolic Imbalance
Metabolic imbalance after liver transplant is
usually of the four types, viz. Hypokalemia, hyperkalemia, hyperglycemia, and
hypomagnesemia, explains a liver surgeon from a top-class liver hospital. For Hypokalemia, supervising the serum potassium level on a regular
basis and supplementation is recommended. For dealing with hyperkalemia, doctors
focus on the dietary changes in the rehabilitation program. Controlling the
CNIs and corticosteroids are helpful to help the patient against the development
of hyperglycemia, diabetic patients are specially looked after. Keeping a check
on the serum magnesium level and supplementation is provided for dealing with
hypomagnesemia.
§ Primary
Non Function
The best bariatric surgeon in Delhi states
the risk of primary nonfunction to be in the range of 4% and 6% following OLT, which has been made possible by the improved methodology of the operation and
post-operative care. If a patient develops primary nonfunction, they showcase
post-transplantation encephalopathy, coagulopathy, minimal bile output,
progressive renal and multisystem failure, increasing serum lactate, and
increasing liver enzyme levels.
§ Portal
Vein Stenosis and Thrombosis
If severe portal vein stenosis and thrombosis
diagnosed after liver transplant, doctors prefer treating the condition or else
it could lead to complete thrombosis of the vein or severe graft dysfunction
and hemodynamic instability secondary to massive ascites.



The article was up to the point and described the information very effectively. Thanks to blog author for wonderful and informative post.
ReplyDeleteLiver Transplant Best Centre